New Releases
Makeup, fragrance-free baby products, travel pouches and more!
Second Skin BB Skin Tint
Regular price from Rs.1,315 -12%
- Unit price
- /per
Baby Lotion
Regular price
Rs.1,795
Rs.1,579
-12%
- Unit price
- /per
Baby Massage Oil
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Baby Eczema Balm
Regular price
Rs.1,895
Rs.1,667
-12%
- Unit price
- /per
Diaper Rash Cream/Balm with Zinc Oxide
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
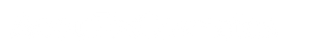
Baby Scalp & Body Wash
Regular price
Rs.2,395
Rs.2,107
-12%
- Unit price
- /per
Encapsulated Retinol + B5 serum
Regular price
Rs.3,195
Rs.2,811
-12%
- Unit price
- /per
Encapsulated Salicylic Acid & Niacinamide Serum
Regular price from Rs.2,371 -12%
- Unit price
- /per
Bestsellers
Most popular with our customers
Powerhouse Serum Vit C, B3, Alpha Arbutin
Regular price
Rs.3,295
Rs.2,899
-12%
- Unit price
- /per
Acne Starter Bundle
Regular price from Rs.5,966 -12%
- Unit price
- /per
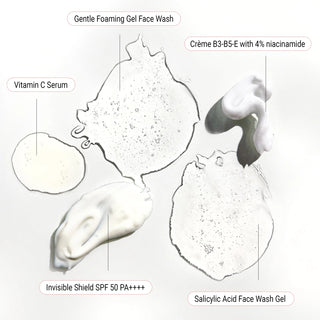
Salicylic Acid Face Wash Gel
Regular price
Rs.1,495
Rs.1,315
-12%
- Unit price
- /per
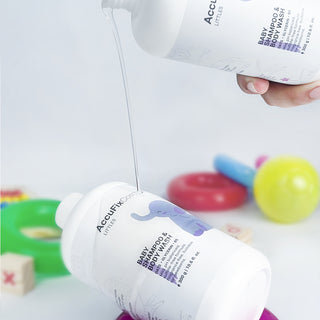
Salicylic Acid Cleanser
Regular price
Rs.1,495
Rs.1,315
-12%
- Unit price
- /per
AHA/BHA Body Wash
Regular price from Rs.1,315 -12%
- Unit price
- /per
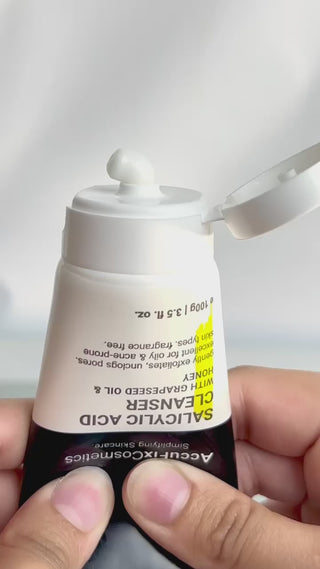
Kojic Acid Glutathione Skin Brightening Cream
Regular price from Rs.1,227 -12%
- Unit price
- /per
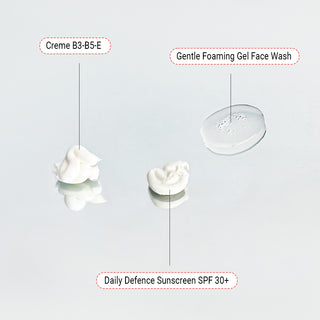
Crème B3-B5-E | 4% Niacinamide Cream
Regular price from Rs.1,227 -12%
- Unit price
- /per
Invisible Shield With Centella SPF 50 PA++++
Regular price
Rs.2,595
Rs.2,283
-12%
- Unit price
- /per
Medicated Anti-Dandruff Salicylic Acid Shampoo
Regular price from Rs.1,315 -12%
- Unit price
- /per
Skin Brightening Bundle
Regular price from Rs.7,550 -12%
- Unit price
- /per
Anti Dandruff Shampoo Bundle
Regular price from Rs.2,499 -12%
- Unit price
- /per
Gel Face Wash Duo
Regular price
Rs.2,790
Rs.2,455
-12%
- Unit price
- /per
Bestselling Body Duo
Regular price from Rs.3,423 -12%
- Unit price
- /per
AccuFix Littles
Safe, unscented baby essentials that you can trust ♥️
Baby Scalp & Body Wash
Regular price
Rs.2,395
Rs.2,107
-12%
- Unit price
- /per
Diaper Rash Cream/Balm with Zinc Oxide
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Baby Eczema Balm
Regular price
Rs.1,895
Rs.1,667
-12%
- Unit price
- /per
Baby Massage Oil
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Baby Lotion
Regular price
Rs.1,795
Rs.1,579
-12%
- Unit price
- /per
Bundles
Curated skin and hair combinations! ♥️
Acne Starter Bundle
Regular price from Rs.5,966 -12%
- Unit price
- /per
Pigmentation Treatment Bundle
Regular price from Rs.12,733 -12%
- Unit price
- /per
Bestselling Body Duo
Regular price from Rs.3,423 -12%
- Unit price
- /per
Lip Pigmentation Bundle
Regular price
Rs.3,785
Rs.3,330
-12%
- Unit price
- /per
3-Step Budget Routine
Regular price
Rs.4,085
Rs.3,594
-12%
- Unit price
- /per
Bestselling Body Duo + Pitti Fresh
Regular price from Rs.5,139 -12%
- Unit price
- /per
Skin Brightening Bundle
Regular price from Rs.7,550 -12%
- Unit price
- /per
Pregnancy Skincare Bundle Routine
Regular price from Rs.5,790 -12%
- Unit price
- /per
Rosacea Treatment Bundle
Regular price from Rs.6,582 -12%
- Unit price
- /per
Anti Dandruff Shampoo Bundle
Regular price from Rs.2,499 -12%
- Unit price
- /per
Gel Face Wash Duo
Regular price
Rs.2,790
Rs.2,455
-12%
- Unit price
- /per
Daily Hair Care Essentials
Regular price from Rs.2,587 -12%
- Unit price
- /per
AccuClear 3-Week Challenge Bundle
Regular price from Rs.10,186 -12%
- Unit price
- /per
Glass Skin Bundle
Regular price from Rs.7,810 -12%
- Unit price
- /per
Cleansers
Gentle, pH-balanced, barrier-friendly formulations.
Salicylic Acid Face Wash Gel
Regular price
Rs.1,495
Rs.1,315
-12%
- Unit price
- /per
Salicylic Acid Cleanser
Regular price
Rs.1,495
Rs.1,315
-12%
- Unit price
- /per
Gentle Foaming Gel Face Wash
Regular price
Rs.1,295
Rs.1,139
-12%
- Unit price
- /per
Hydrating Gentle Daily Cleanser
Regular price
Rs.1,495
Rs.1,315
-12%
- Unit price
- /per
Butter But Better Cleansing Balm | Makeup Remover
Regular price
Rs.1,395
Rs.1,227
-12%
- Unit price
- /per
Resurfacing Face Wash with turmeric & honey
Regular price
Rs.1,745
Rs.1,535
-12%
- Unit price
- /per
Treatments
Potent products to target specific skin concerns.
Encapsulated Salicylic Acid & Niacinamide Serum
Regular price from Rs.2,371 -12%
- Unit price
- /per
Encapsulated Retinol + B5 serum
Regular price
Rs.3,195
Rs.2,811
-12%
- Unit price
- /per
Powerhouse Serum Vit C, B3, Alpha Arbutin
Regular price
Rs.3,295
Rs.2,899
-12%
- Unit price
- /per
Oat and Glycolic Acid Gel Toner
Regular price
Rs.2,295
Rs.2,019
-12%
- Unit price
- /per
Azelaic Acid Serum
Regular price
Rs.3,395
Rs.2,987
-12%
- Unit price
- /per
Salicylic Acid Serum | BHA Serum
Regular price
Rs.2,095
Rs.1,843
-12%
- Unit price
- /per
Niacinamide Serum | Niacin Serum
Regular price
Rs.2,095
Rs.1,843
-12%
- Unit price
- /per
Salicylic Acid Cream
Regular price
Rs.2,095
Rs.1,843
-12%
- Unit price
- /per
Retin-oil Serum 0.2%-1.0% | Best Retinol Serum
Regular price from Rs.2,107 -12%
- Unit price
- /per
Vitamin C Serum with 10% SAP
Regular price
Rs.2,095
Rs.1,843
-12%
- Unit price
- /per
100% Pure, Organic Wild Sea Buckthorn Oil
Regular price
Rs.3,495
Rs.3,075
-12%
- Unit price
- /per
Hydrocolloid Pimple Patches | Acne Patches
Regular price
Rs.1,200
Rs.1,056
-12%
- Unit price
- /per
Moisturisers
Non-comedogenic options to fortify your skin barrier.
Kojic Acid Glutathione Skin Brightening Cream
Regular price from Rs.1,227 -12%
- Unit price
- /per
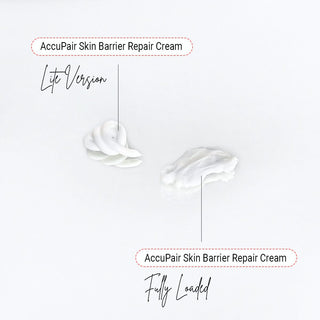
AccuPair Skin Barrier Repair Cream
Regular price from Rs.2,195 -12%
- Unit price
- /per
Crème B3-B5-E | 4% Niacinamide Cream
Regular price from Rs.1,227 -12%
- Unit price
- /per
AccuHydra Hydrating Gel Crème
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Carbamide Intensive Hydration Cream
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Medium Chain Triglyceride (M.C.T.) Oil
Regular price
Rs.1,295
Rs.1,139
-12%
- Unit price
- /per
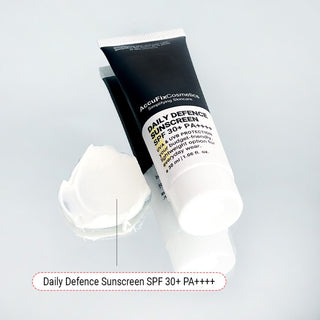
Sunscreens
Bestselling options you'll actually want to wear.
Invisible Shield With Centella SPF 50 PA++++
Regular price
Rs.2,595
Rs.2,283
-12%
- Unit price
- /per
The Ultimate Sunscreen SPF 50+ PA++++
Regular price
Rs.1,995
Rs.1,755
-12%
- Unit price
- /per
Daily Defence Sunscreen SPF 30+ PA+++
Regular price
Rs.1,395
Rs.1,227
-12%
- Unit price
- /per
Lip Protection Balm SPF 30+ PA++++
Regular price
Rs.1,295
Rs.1,139
-12%
- Unit price
- /per
Colour Changing UV Detection Stickers
Regular price
Rs.1,200
Rs.1,056
-12%
- Unit price
- /per
Lip Care
Product designed especially for delicate lip skin.
Lip Pigmentation Bundle
Regular price
Rs.3,785
Rs.3,330
-12%
- Unit price
- /per
Lip Treatment Balm
Regular price
Rs.890
Rs.783
-12%
- Unit price
- /per
Dark Lips Treatment Balm
Regular price
Rs.1,395
Rs.1,227
-12%
- Unit price
- /per
Lip Protection Balm SPF 30+ PA++++
Regular price
Rs.1,295
Rs.1,139
-12%
- Unit price
- /per
The Unscrub Lip Scrub with Glycolic Acid
Regular price
Rs.1,095
Rs.963
-12%
- Unit price
- /per
Beauty Tools & Accessories
From pimple patches to electric tools that level up your personal care.
Hydrocolloid Pimple Patches | Acne Patches
Regular price
Rs.1,200
Rs.1,056
-12%
- Unit price
- /per
Bamboo Charcoal Konjac Sponge
Regular price from Rs.1,056 -12%
- Unit price
- /per
Makeup Zipper Pouch
Regular price
Rs.1,695
Rs.1,491
-12%
- Unit price
- /per
Colour Changing UV Detection Stickers
Regular price
Rs.1,200
Rs.1,056
-12%
- Unit price
- /per
Multi-Modal Electronic Gua Sha
Regular price
Rs.9,999
Rs.7,999
-20%
- Unit price
- /per
Foldable Travel Cosmetic Pouch
Regular price
Rs.2,995
Rs.2,635
-12%
- Unit price
- /per
Hair Care
Formulated with hair and scalp health in mind.
Medicated Anti-Dandruff Salicylic Acid Shampoo
Regular price from Rs.1,315 -12%
- Unit price
- /per
Clarify & Rebalance Shampoo
Regular price from Rs.1,183 -12%
- Unit price
- /per
Rosemary Oil Hair Fall Treatment
Regular price
Rs.2,695
Rs.2,371
-12%
- Unit price
- /per
Frizz Control & Shine Hair Serum
Regular price
Rs.1,795
Rs.1,579
-12%
- Unit price
- /per
Strength & Shine Hair Conditioner
Regular price from Rs.1,403 -12%
- Unit price
- /per
Damage Repair Protein Hair Mask
Regular price
Rs.2,695
Rs.2,371
-12%
- Unit price
- /per
Anti Dandruff Shampoo Bundle
Regular price from Rs.2,499 -12%
- Unit price
- /per
Body Care
To target body acne, dark patches, KP and more!
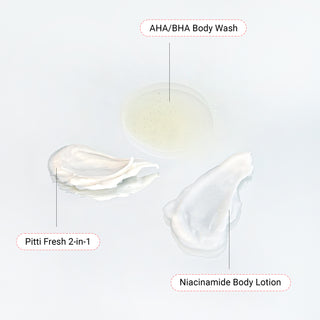
AHA/BHA Body Wash
Regular price from Rs.1,315 -12%
- Unit price
- /per
Niacinamide Body Lotion
Regular price
Rs.2,395
Rs.2,107
-12%
- Unit price
- /per
Pitti-Fresh 2-in-1 Underarm Lightening Deo Cream
Regular price
Rs.1,950
Rs.1,716
-12%
- Unit price
- /per
Skin Repair Balm | Eczema, Cracked Heels
Regular price
Rs.2,395
Rs.2,107
-12%
- Unit price
- /per
Bestselling Body Duo
Regular price from Rs.3,423 -12%
- Unit price
- /per